How CCTA Can Inform LDL Treatment
“To lose patience is to lose the battle.”
– Mahatma Gandhi
Throughout clinical medicine, the question of early intervention versus judicious waiting drives outcomes for our patients. While a patient may be anxious for action, clinical data has demonstrated that the tradeoffs associated with action vs conservative approaches can sometimes result in minimal benefits or even in harm from early intervention. Restraining well-intentioned desires to take action requires discipline.
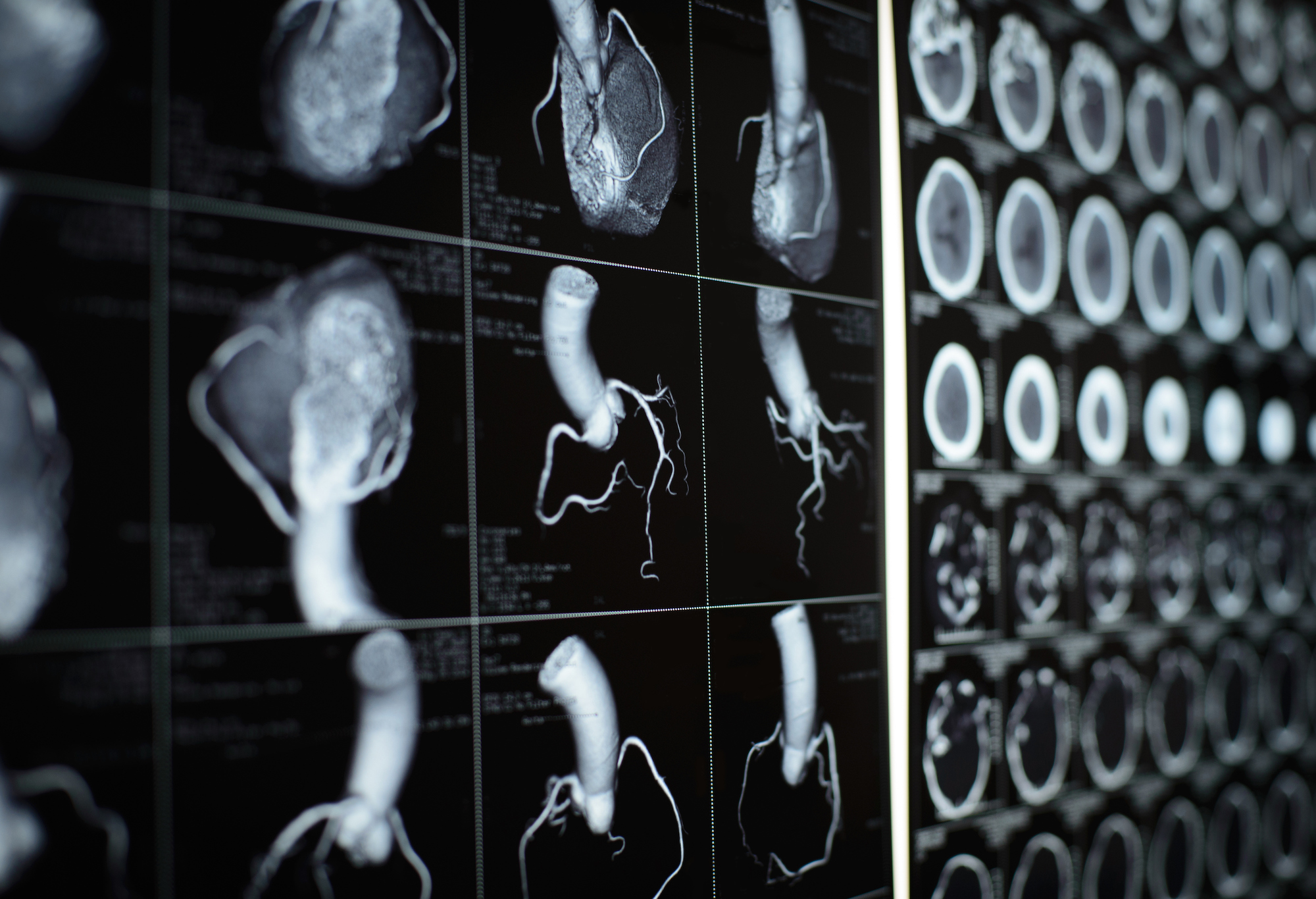
Within cardiology, the increased utilization of coronary CT angiography (CCTA) has historically been largely used to justify a decision to defer action. With its unparalleled ability to identify disease, clinicians can confidently rule out coronary artery disease (CAD) in patients with a normal CCTA.
However, I was struck by a recent publication that highlighted how CCTA can inform clinicians about when to take action, specifically with regards to lowering LDL to ESC and ACC/AHA guideline targets. Dr. M. B. Mortensen and colleagues in Denmark demonstrated that CCTA can be used to inform this common clinical decision.
Since 2013, when the ACC and AHA expanded guidelines to recommend new targets for LDL lowering, there have been significant questions as to whether these important treatment choices would be over-prescribed. Many prominent leaders have argued that “statins provide false assurances that may discourage patients from taking the steps that actually reduce cardiovascular disease.”
Dr. Mortensen’s work informs this debate beyond prior studies. In a population of over 20,000 symptomatic patients who underwent CCTA, and then were followed for six years or until a clinical event, a strong inverse relationship was described between increasing CAD burden on CCTA and a more favorable (i.e., lower) number of patients requiring lowering LDL to ESC and ACC/AHA guideline targets in order to prevent an event (NNT).
For example, among patients with a normal CCTA, reaching guideline-targets was not expected to yield significant patient benefits. At least 110 patients with a normal CCTA would have to be treated to ACC/AHA targets for six years to prevent a single clinical event. This is in sharp contrast to the population of patients with three-vessel CAD on CCTA, among whom just nine patients would need to undergo such treatment to prevent one coronary event.
Most importantly, by better targeting the medical approach to LDL lowering, the overall number of adverse coronary events can be reduced: over one out of three events prevented in patients with obstructive CAD and up to one out of four in patients with non-obstructive CAD.
“An individualized approach based on CAD severity can identify symptomatic patients that are likely to derive most and least benefit from [statin initiation].” These CCTA-driven, personalized decisions enable better-informed conversations with patients and avoidance of “false assurances” that intervention rather than waiting is in every patient’s best interest.
— A perspective from HeartFlow Chief Medical Officer, Campbell Rogers, MD
Bio | LinkedIn





